Vicky Foxcroft MP for Lewisham Deptford & Shadow Minister for Disabled People
To mark the first ever Neonatal Mental Health Awareness Week (launched by neonatal charity Leo’s), I asked my office manager, Vicki, to share her experiences of having a premature baby. It is clear that the Government needs to do more to ensure that parents have access to mental health support at what can be an incredibly stressful time.
In 2015 my son was born at just over 24 weeks’ gestation, weighing a tiny 715g. It came as a massive shock: although it later became clear that his birth had been precipitated by an infection, the midwives I had seen the evening before diagnosed me with dehydration and told me I just needed fluids. A few hours later he arrived by (very) emergency caesarean under general anaesthetic.
Although the staff at our local hospital did an amazing job of caring for him in his first few hours, the special care baby unit is only equipped to support babies born at a later gestation. So at around seven hours old, our tiny boy was transferred to the fantastic Neonatal Intensive Care Unit the Evelina Children’s Hospital, where he stayed for 5.5 weeks before being transferred back. He finally came home on day 109.
Overall, we had a pretty easy ride. There were definite troughs – including two infections and a diagnosis of retinopathy of prematurity which required surgery – but all in all we felt we had escaped relatively unscathed. I include myself and my partner in that: although our experience was incredibly difficult at times, we felt that we were relatively unaffected by it from an emotional point of view. We had bonded with the staff at both hospitals, felt involved in our son’s care and were always encouraged to speak about our concerns. We also formed friendships with other parents, which continue to this day.
However, once the initial euphoria of escaping the hospital had worn off, I found I had frequent flashbacks to the birth and the darker times we had experienced. I still do now, albeit with longer periods in between. And I often reflect on the ‘survivor guilt’ we have been left with; at the most unexpected moments a song or tv show can trigger thoughts of all the families who didn’t get to take their babies home.
Very few parents expect to end up in NICU. Some may have a certain amount of warning (ranging from a few days to several weeks in the case of friends), but others, like us, have no warning at all. No matter how resilient we think we are, it is bound to have an impact on our mental health.
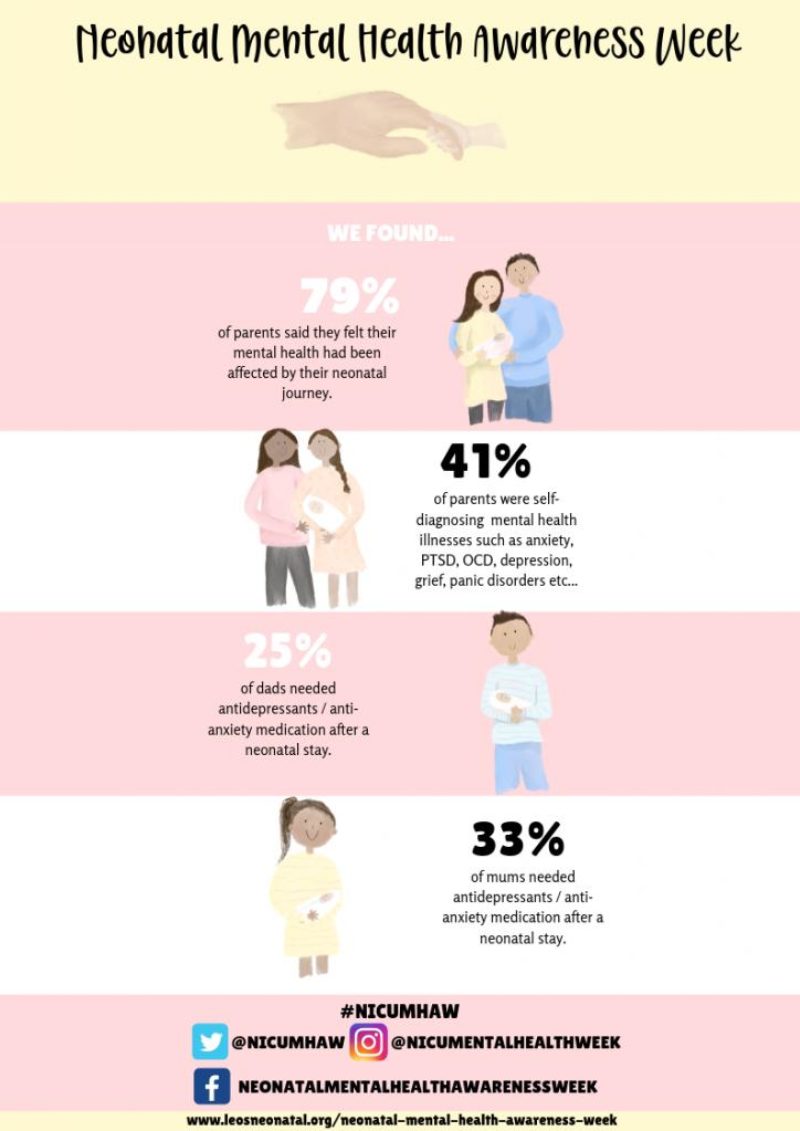
Research carried out last year by Bliss, a charity which supports parents and staff in neonatal units, found that a massive 80% of parents believed their mental health had suffered after their neonatal experience. 39% felt that they had actually developed a mental health condition as a result and a worrying 62% reported that they had no access to psychological support. Further research carried out by Leo’s reported very similar numbers.
Parents and families are not only affected by the medical side of things. Worries about money, work, other children and simply managing day-to-day life can quickly lead to a downturn in mental health. I was very lucky to have a supportive boss and colleagues who did everything they could to ensure I didn’t worry about work, but not everyone is as fortunate. Vicky could not, however, do anything about the fact that my maternity leave kicked in straightaway and I missed out on almost four months of the time I had planned to spend at home.
In November 2017 we asked the Secretary of State for Health, what progress his department had made towards ensuring that all parents and staff on neonatal units have access to psychological support in line with national standards. The minister who responded, Jackie Doyle-Price MP, advised that the Government’s Five Year Forward View for Mental Health includes a specific recommendation to improve perinatal mental health services and that “the aim is that by 2020/21, there will be increased access to specialist perinatal mental health support in all areas of England.” We have tabled a question this week to ask for an update on the progress that has been made.
Charities such as Bliss, which has a telephone support line for parents and volunteers working in hospitals, do an incredible job. But the Government must continue to acknowledge the lifelong implications of poor parental mental health. It is recognised as one of the Acute Childhood Experiences which are strongly associated with high risk health behaviours in adulthood and if our children are not supported from the very beginning, it can have lifelong consequences.
Neonatal Mental Health Awareness Week runs from 15th-21st April 2019.